
Breast reduction surgery, or reduction mammaplasty, is a significant surgical procedure aimed at reducing the size and weight of large breasts. This operation addresses both physical discomfort and aesthetic concerns, enhancing the overall quality of life for patients. The following sections detail the fundamental aspects of breast anatomy important for surgical planning, discuss the medical reasons prompting such interventions, and describe various surgical techniques to tailor the procedure to individual needs.
This guide also covers essential operative considerations, such as the effective use of infiltration techniques to minimize blood loss and the role of postoperative drains in recovery. Additionally, it provides a comprehensive overview of potential complications and their management strategies. Whether refining surgical skills or updating knowledge on current practices, this article is a thorough resource for healthcare professionals involved in breast reduction surgeries.
Key Aesthetic Parameters of Breast Anatomy
A thorough comprehension of the normal aesthetics of the breast is important for clinical evaluations and cosmetic procedures. The details below describe the essential anatomical features and proportions that characterize an aesthetically appealing breast. These guidelines help assess and plan surgical enhancements to achieve medically appropriate outcomes that are visually harmonious with the individual's body.
- Position and Symmetry: Breasts should exhibit symmetry, with the nipple-areola complex (NAC) optimally positioned on the most projecting part of each breast mound. The NAC should align with Pitanguy's point, located at the intersection of the mid-clavicular line and a horizontal line at the level of the fourth intercostal space.
- Size and Shape: Proportional to the individual's body size, the breast contour should adhere to the classic Penn numbers: 21 cm from the sternal notch to the nipple and 6.9 cm from the nipple to the inframammary fold (IMF). Some patients potentially require a notch-to-nipple distance of 22-24 cm and a nipple-to-IMF distance of 10-12 cm for optimal shaping.
- Nipple-Areola Complex (NAC): The NAC should be round or oval, ideally between 38-45 mm in diameter, facing forward or slightly outward, with a slight upward tilt at a 10-20 degree angle relative to the horizontal plane.
- Inframammary Fold (IMF): The IMF should be well-defined, forming a gentle curve consistent with the overall breast shape, and positioned to support the breast adequately without causing excessive skin tension.
- Skin Quality: The skin of the breasts should be smooth and taut, appropriately reflecting the individual's age and health, with minimal blemishes or signs of ptosis.
- Breast Root: The width of the breast root should harmonize with the thoracic dimensions, ensuring that the breasts are neither too wide nor too narrow for the chest, contributing to a balanced aesthetic appearance.
Pathophysiology of Hypermastia
Hypermastia, often termed macromastia, is characterized by an abnormal enlargement of the breasts. This condition arises from a complex interplay of hormonal, genetic, and environmental factors that drive excessive breast tissue growth.
- Hormonal Dynamics: While estrogen levels may remain normal, the breast tissues show an abnormal growth response to these circulating estrogens, possibly due to increased estrogen receptors.
- Tissue Composition: The enlargement is primarily due to an increase in fibrous tissue and adipose tissue, with a relatively smaller increase in glandular tissue.
- Genetic Influence: Genetics may predispose individuals to hypermastia, affecting how breast tissue responds to normal hormonal levels.
- Adipose Tissue Contribution: Fat tissue accumulation within the breasts can significantly contribute to their size, particularly in cases of general obesity.
- Systemic Conditions: Conditions such as hypothyroidism can influence breast size indirectly through their hormonal effects on the body.
A History of Breast Reduction Surgery
Bread reduction surgery, more commonly known as breast reduction surgery or reduction mammaplasty, is a surgical procedure aimed at reducing the size and weight of large breasts to alleviate associated physical discomforts. This operation has evolved significantly over the years, integrating advances in surgical techniques and patient care.
Early Techniques
- Thorek (1920s): Introduced the free nipple graft technique, marking an early approach to addressing large reductions where nipple preservation was challenging.
Development of Pedicle Methods
- Wise (1950s): Developed the keyhole pattern of skin incision for reshaping the breast.
- Strombeck (1960): Introduced the horizontal bipedicle technique.
- Skoog (1963): Proposed the superomedial pedicle technique, modifying Strombeck's approach.
- McKissock (1972): Created the vertical bipedicle technique.
- Weiner (1973): Developed the superior pedicle technique.
- Ribeiro (1975): Introduced the inferior pedicle technique, which preserves the nipple and areola's blood supply and sensation.
Integration of Liposuction
- 1980s: Liposuction was introduced as an adjunct to traditional excision methods in breast reduction, allowing for less invasive fat removal with reduced scarring and quicker recovery times.
Evolution of Vertical Scar Techniques
- Lejour: Popularized the vertical scar technique, originally described by Lassus.
- Hall-Findlay (1999): Modified the vertical scar technique with a medial pedicle.
- Hammond (1999): Developed the short scar periareolar inferior pedicle reduction (SPAIR) technique.
Introduction of the Round-Block Technique
- Benelli (1990): Introduced the round-block technique, focusing on periareolar incisions to reduce scarring.
Recent Innovations
- Hamdi (2005): Used the septum of Würinger to maintain vascularity and sensation to the nipple–areola complex (NAC), further enhancing the technical sophistication of breast reductions.
Refinement and Customization
- Surgeons now often employ a combination of methods tailored to individual anatomical needs and patient expectations, focusing on refining techniques to enhance aesthetic outcomes and reduce recovery time.
Technological Advances
- Technology, including 3D imaging and endoscopic assistance, has improved pre-surgical planning and precision, leading to more consistent and satisfactory results.
Indications for Breast Reduction Surgery
Breast reduction surgery, or reduction mammaplasty, is performed to address physical and psychological issues arising from excessively large breasts. This procedure alleviates discomfort and improves the patient's quality of life and body image.
- Chronic Pain: Persistent back, neck, and shoulder pain due to the weight of large breasts.
- Physical Limitations: Reduced ability to engage in physical activities, leading to a sedentary lifestyle.
- Skin Irritations: Issues such as intertrigo under the breast crease caused by excess moisture and friction.
- Postural Problems: Poor posture and potential spinal deformities resulting from the strain of supporting heavy breasts.
- Respiratory Distress: Breathing difficulties that may occur due to the excessive chest weight.
- Psychological Impact: Negative effects on mental health, including body image disturbances and social embarrassment.
- Disproportionate Breast Size: Breasts that are disproportionately large compared to the rest of the body, affecting aesthetic appearance and clothing fit.
Breast Reduction Surgical Techniques
Breast reduction surgery incorporates diverse methods characterized by skin excision patterns and nipple-areola complex (NAC) pedicle designs. Selecting a specific technique depends on the patient's unique anatomical features, the desired reduction, and the technique's potential for achieving optimal aesthetic and functional outcomes.
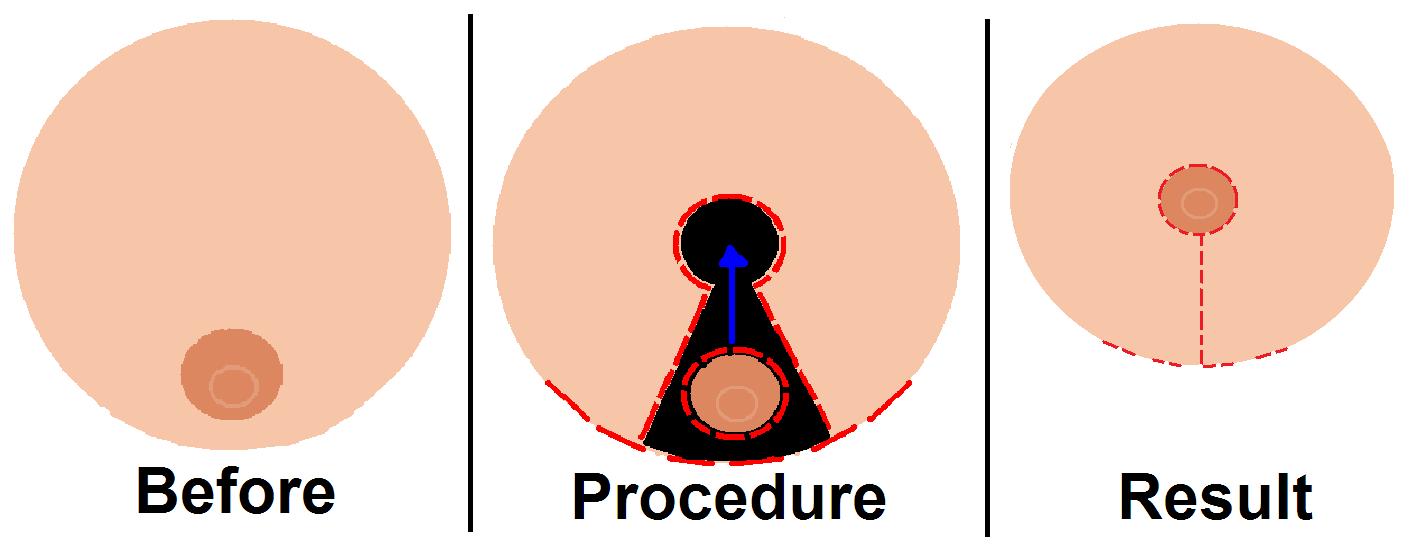
Wise Pattern (Inverted T/Keyhole)
- Skin Excision: Employed for extensive tissue removal, accommodating larger reductions with a classic anchor-shaped or keyhole incision.
- NAC Pedicle: Generally inferior, ensures robust blood flow and sensory preservation, and can support large resections.
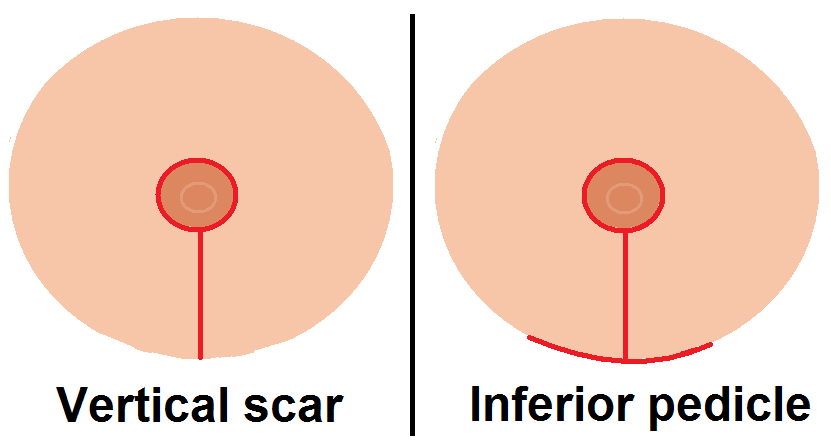
Vertical Pattern
- Skin Excision: Features a vertical incision from the areola to the inframammary fold, with variations including short lateral extensions for better contouring, popularized by Lejour and Marchac.
- NAC Pedicle: Often involves superior or medial pedicles, facilitating breast projection while minimizing scarring.
Periareolar (Benelli)
- Skin Excision: Centers on a periareolar incision, ideal for minor reductions and aesthetic enhancements, limiting scarring to around the areola.
- NAC Pedicle: Can be composed of glandular tissue alone or in combination with de-epithelialized dermis, minimizing visible scarring while maintaining central vascularity.
Free Nipple Graft
- Skin Excision: Extensive, necessary in cases requiring significant reductions where the NAC's vascular integrity might be at risk.
- NAC Pedicle: None, with the NAC entirely removed and regrafted, typically used for patients with very long nipple-to-IMF distances or those with compromised vascularity.
Inferior Pedicle Technique
- Skin Excision: Often adopts an inverted-T pattern suited for substantial volume management.
- NAC Pedicle: Maintains attachment to the chest wall, often adjusted to include sensory branches, which is crucial for sensory preservation and vascular robustness.
Medial Pedicle Technique
- Skin Excision: Generally utilizes a vertical incision that diminishes horizontal scarring.
- NAC Pedicle: Constructed as a full-thickness dermoglandular pedicle, ensuring a high level of NAC sensation and blood supply, appearing superomedial when the patient is upright.
Ultrasound-Assisted and Suction Lipectomy
- Skin Excision: Minimal, with incisions primarily for cannula entry, focusing on fat removal rather than extensive tissue excision.
- NAC Pedicle: Not repositioned; these techniques are preferred in patients with fatty breasts and less concern for dramatic reshaping but significant volume reduction and minimal scarring.
Lateral Pedicle
- Skin Excision: Adapted based on specific patient needs, typically less extensive.
- NAC Pedicle: Based on lateral thoracic artery perforators, noted for improving NAC vascularization and sensation, especially effective in creating shorter pedicles for extensive reductions.
Infiltration Techniques in Breast Reduction Surgery
Infiltration during breast reduction surgery is a key technique that involves administering dilute solutions into the surgical site to minimize blood loss and enhance procedural efficiency. This approach is widely recognized for its effectiveness in improving surgical outcomes.
- Purpose: Primarily aimed at reducing operative blood loss and providing localized pain control, diminishing the need for systemic analgesics during and after surgery.
- Common Solutions: Solutions often contain a combination of local anesthetics and epinephrine. A common formulation is 0.25% prilocaine with 1:800,000 epinephrine or even more dilute forms such as 1:1,000,000 epinephrine.
- Method of Application: The solution is typically injected into the retroglandular space and along the planned incision lines using fine cannulas or needles to ensure targeted application.
- Volumes and Concentrations: Specific volumes include 40 ml per breast, divided equally between the retroglandular space and incision lines, with variations based on surgical scope and patient-specific factors.
- Efficacy: Studies, such as those by Wilmink and Samdal, have demonstrated significant reductions in intraoperative blood loss, with treated breasts showing less than 50% blood loss compared to untreated controls. Infiltration has also been shown to reduce operative time and postoperative recovery duration.
- Technique Variations: Utilized in various breast reduction patterns such as superomedial pedicle, inferior pedicle, and McKissock (bipedicle), confirming its versatility across different surgical approaches.
- Outcomes: The use of infiltration has no significant impact on skin flap viability, postoperative drainage, or operation duration, indicating that its benefits in blood loss reduction and pain control do not compromise surgical safety or recovery.
Postoperative Drains in Breast Reduction Surgery
Recent studies have questioned the necessity and effectiveness of postoperative drains in breast reduction surgery. While traditionally used to prevent fluid accumulation and complications, emerging evidence suggests their utility may be limited.
- Purpose Reevaluated: Drains are intended to prevent complications like hematomas and seromas by removing excess fluids, but recent studies challenge their effectiveness in lowering complication rates.
- Recent Findings:
- Studies by Wrye et al. and Corion et al. observed no significant difference in complication or hematoma rates between drained and undrained breasts in patients undergoing breast reduction.
- Matarasso et al. found no increased complication rates in surgeries performed without drains, suggesting that routine drain use may not be necessary.
- Types and Placement: Silicone drains such as Jackson-Pratt or Blake are typically used strategically within the surgical site. Complication Rates: Corion et al. reported a higher overall complication rate in patients with drains than in those without (40% vs. 23%).
- Output Monitoring: Although drains are managed based on output volume, Ngan et al. concluded that patients under 50 with resections under 500 grams might not need drains.
- Management and Removal:
- Drains are usually kept for 1 to 3 days postoperatively. Removal criteria include an output of less than 30 ml over 24 hours.
- Education on drain care remains crucial for patients who do have drains placed.
Complications in Breast Reduction Surgery
Breast reduction surgery, while highly effective in alleviating symptoms associated with large breasts, carries potential risks and complications. Awareness and early identification are crucial for effective management.
- Hematoma: Accumulation of blood inside the breast tissue, often requiring surgical intervention to drain and resolve.
- Seroma: Formation of fluid-filled pockets post-surgery, typically managed with aspiration or additional drainage if persistent.
- Infection: Risk of bacterial infection at the incision sites, requiring antibiotics and sometimes surgical cleaning.
- Scarring: Although scars are inevitable in surgery, poor healing can lead to hypertrophic or keloid scars. Unsatisfactory scarring affects about 4% of patients.
- Changes in Nipple Sensation: Temporary or permanent changes in nipple sensitivity, including numbness or heightened sensitivity. Altered sensation occurs in 9%-25% of patients, more frequently with larger amounts of tissue resection.
- Nipple Necrosis: Partial or total loss of the nipple due to compromised blood supply, occurring in 4%-7% of patients.
- Asymmetry: Differences in size, shape, or nipple position between the breasts post-surgery.
- Fat Necrosis: The death of fat cells in the breast tissue, which can cause firm lumps and sometimes pain.
- Breastfeeding Difficulties: Reduction surgery can affect breastfeeding ability, impacting glandular tissue and ducts. The ability to breastfeed postoperatively varies, with many patients requiring supplemental feeding.
- Aesthetic Dissatisfaction: Some patients may be unhappy with the outcome regarding breast size, shape, or symmetry.
- Wound-Healing Complications: Up to 19% of patients experience issues ranging from minor delays to significant complications requiring additional interventions.

Courses are
coming soon...
Our aim is to comprehensively cover every specialty within medicine, bringing you courses that provide value and aid your professional growth.

